Comprehensive eye exams are the bread and butter for every optometrist, regardless of the setting. Though patient demographics and chief complaints may be different, the core of everything we do and the testing we perform remains the same. All of the testing we perform on a daily basis in clinic is essential, but sometimes it’s hard to prioritize what to do and when to do it when it comes to looking for something specific or finding evidence for a certain diagnosis.
Given the prevalence of diabetes in the world, regardless of population and demographic, it’s important to develop a flow for your diabetic eye exam to ensure you never miss a step and to triage your patient properly. Below are some tests that we do perform on a daily basis, and here we will elaborate on how paying close attention to this testing will give us a clearer understanding of the patient’s diabetic state, as well as the necessity for referral or intervention.
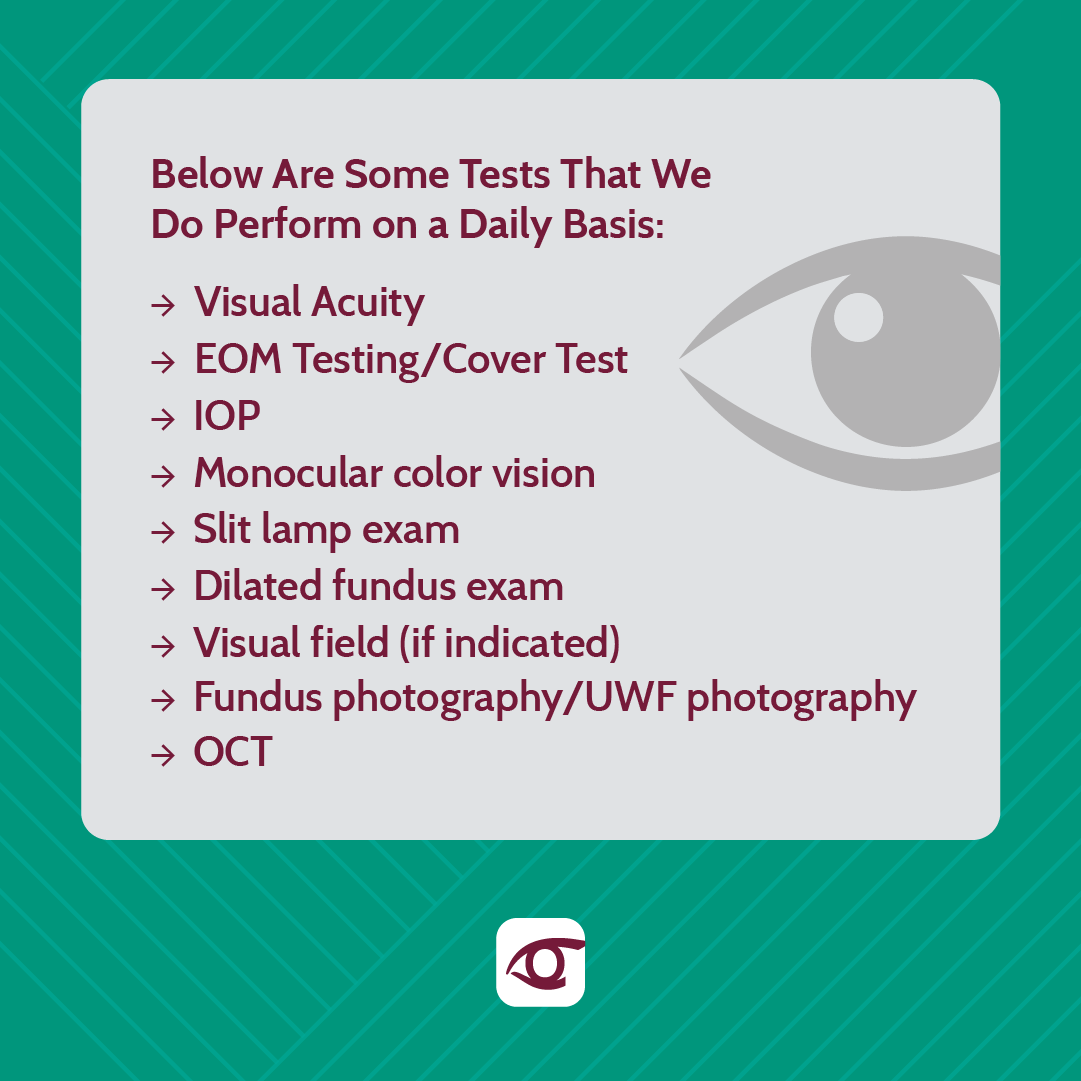
Visual Acuity: Of course, every patient that enters your exam room has their visual acuity taken. However, comparing best corrected visual acuity year after year will give you a great idea of possible progression, blood sugar fluctuations, or early cataract development. If your patient is new and something doesn't make sense, try to request previous patient records that will give you some information for comparison.
EOM Testing/Cover Test: This step is overlooked in adults and emphasized in children. However, diabetes can lead to neurological disorders and cranial nerve palsies. Therefore, evaluation of the extraocular muscles and eye alignment is important year after year, in case the patient develops a palsy down the line.
IOP: Your diabetic patients are more likely to develop glaucoma. Checking IOP is critical to determine if additional testing for glaucoma will be indicated.
Monocular color vision: Studies show that color vision may be affected in patients with diabetes, even in the absence of retinopathy. Checking color vision monocularly can give you an understanding of which eye may develop retinopathy faster!
Slit lamp exam: Pay close attention to the iris for any neovascularization and the crystalline lens for any nuclear changes!
Dilated fundus exam: This step should be self explanatory. Performing a dilated fundus exam is critical in patients with diabetes. However, don’t get stuck on the fundus. Always remember to check the peripheral retina as well!
Visual field (if indicated): This is important in patients with a cataract who are not best correctable to 20/20 or patients with advanced disease and a history of surgical/laser intervention. Patients who have had pan-retinal photocoagulation can show visual field defects corresponding to the peripheral visual field.
Fundus photography/UWF photography : This is the best tool for photo documentation and patient education!
OCT: In the presence of macular edema, a macular OCT can give you a good idea of severity and a basis for referral.
Critical thinking and putting all of the pieces to the puzzle together during a diabetic eye exam will help you build efficient referral and patient management patterns. Remember to network in your area with retina specialists and collaborate with them on protocols and patient care to ensure a seamless transition and patient compliance.
Dr. Amadian
