Optometrists are often on the front-line when it comes to diagnosis of certain medical conditions, as many disorders can present with ocular signs and symptoms as the initial indicators of disease. With that being said, there are a few conditions that you don’t want to miss as the first physician to see the patient; an acquired third nerve palsy is one of them.
Here we will review the differences between pupil-sparing and pupil-involving oculomotor nerve palsies, as an acquired pupil-involving 3rd nerve palsy is considered one of the true serious emergencies in neuro-optometry.
Clinical findings associated with an acquired oculomotor nerve palsy can vary greatly depending on the location of the lesion along the course of the nerve. Cranial nerve III palsies can be divided into either a partial or complete palsy.
Complete 3rd nerve palsies will present with a complete eyelid ptosis with the eye in a downward and outward position and the inability to adduct, infraduct, or supraduct. Patients will also have a dilated pupil with sluggish reaction to light. Partial 3rd nerve palsies are more common than complete palsies and can present with variable duction limitations of the affected extraocular muscles and varying degrees of eyelid ptosis and/or pupillary dysfunction.
Acquired oculomotor nerve palsy can occur secondary to many different etiologies. If a patient presents to your office with ophthalmoplegia, ptosis, and mydriasis, a compressive etiology, such as an intracranial aneurysm must be ruled out.
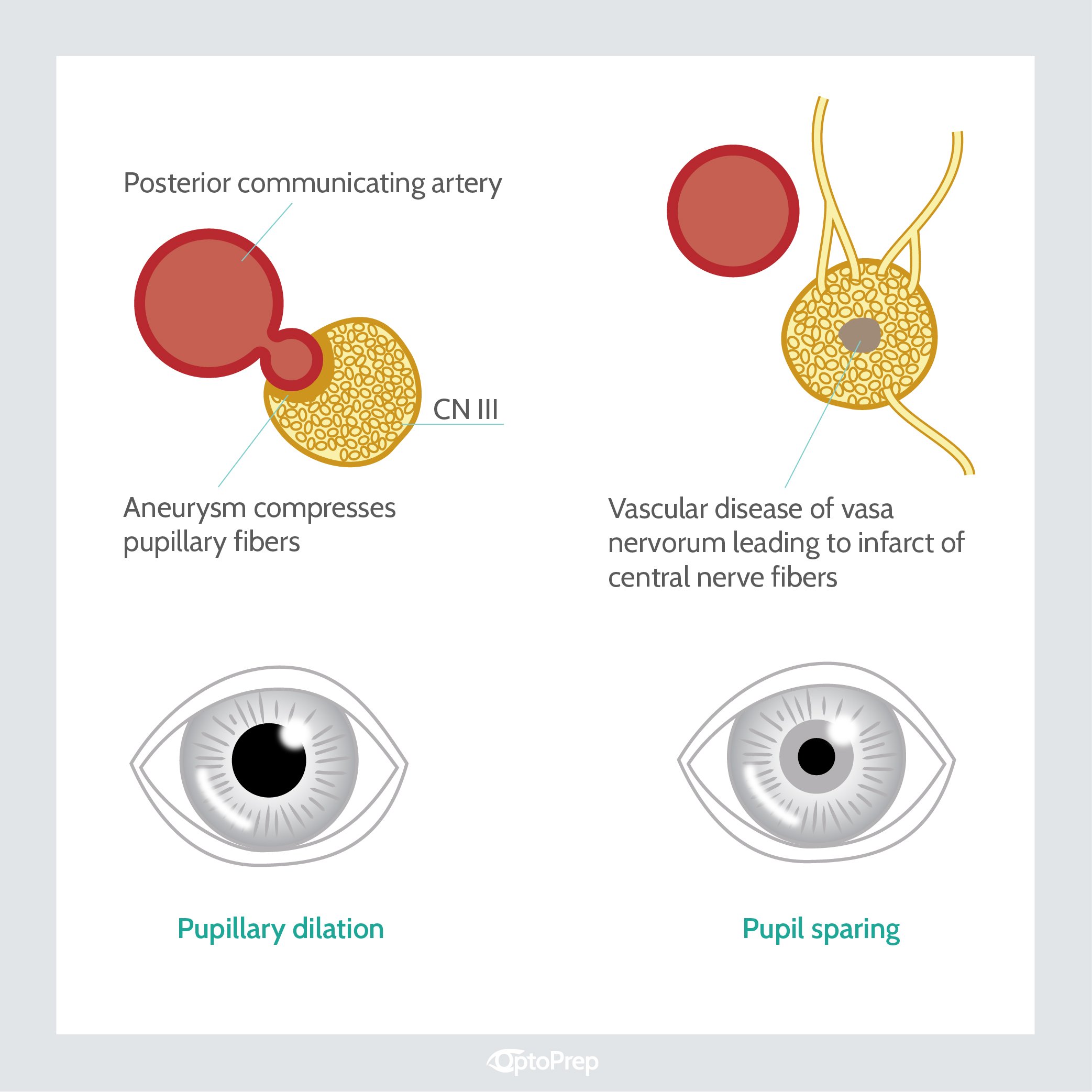
It is important to remember that pupillary fibers occupy a peripheral location within the oculomotor nerve and receive more collateral blood supply than that of the main trunk of the nerve. It is for this reason that these fibers are more susceptible to compressive lesions. The most commonly known etiology in this case is a posterior communicating artery aneurysm.
If the patient presents with a complete or incomplete oculomotor palsy without pupil involvement (pupil-sparing 3rd nerve palsy), it is most likely related to ischemic processes (but compression and inflammation should still be considered).
SPECIAL OFFER:
Sign up for a 90-day Part II OptoPrep subscription before
midnight this Friday and receive 10% off!
Use promo code: OP2FlashSale
As mentioned above, pupillary fibers run peripherally within the nerve and receive more collateral blood supply; therefore, these fibers are less susceptible to ischemia. Evaluation and management will vary according to the patient’s medical history, age, and associated symptoms; however, a basic work-up must be completed on all patients to determine the etiology of ischemia.
These tests should include: vital signs, complete blood count (CBC), erythrocyte sedimentation rate (ESR), and a comprehensive metabolic panel (CMP).
Most of these patients typically show improvement after the first 4 weeks, with full resolution occurring within 12 weeks of the insult.
Bottom line
Be vigilant in making the diagnosis and referring out immediately to determine the underlying cause. If a compressive lesion is suspected, get your local neuro-ophthalmologist on the phone and coordinate sending the patient for urgent imaging. These cases are rare, but you never know when one might sit down in your chair, so be ready! You just may save someone’s life!
