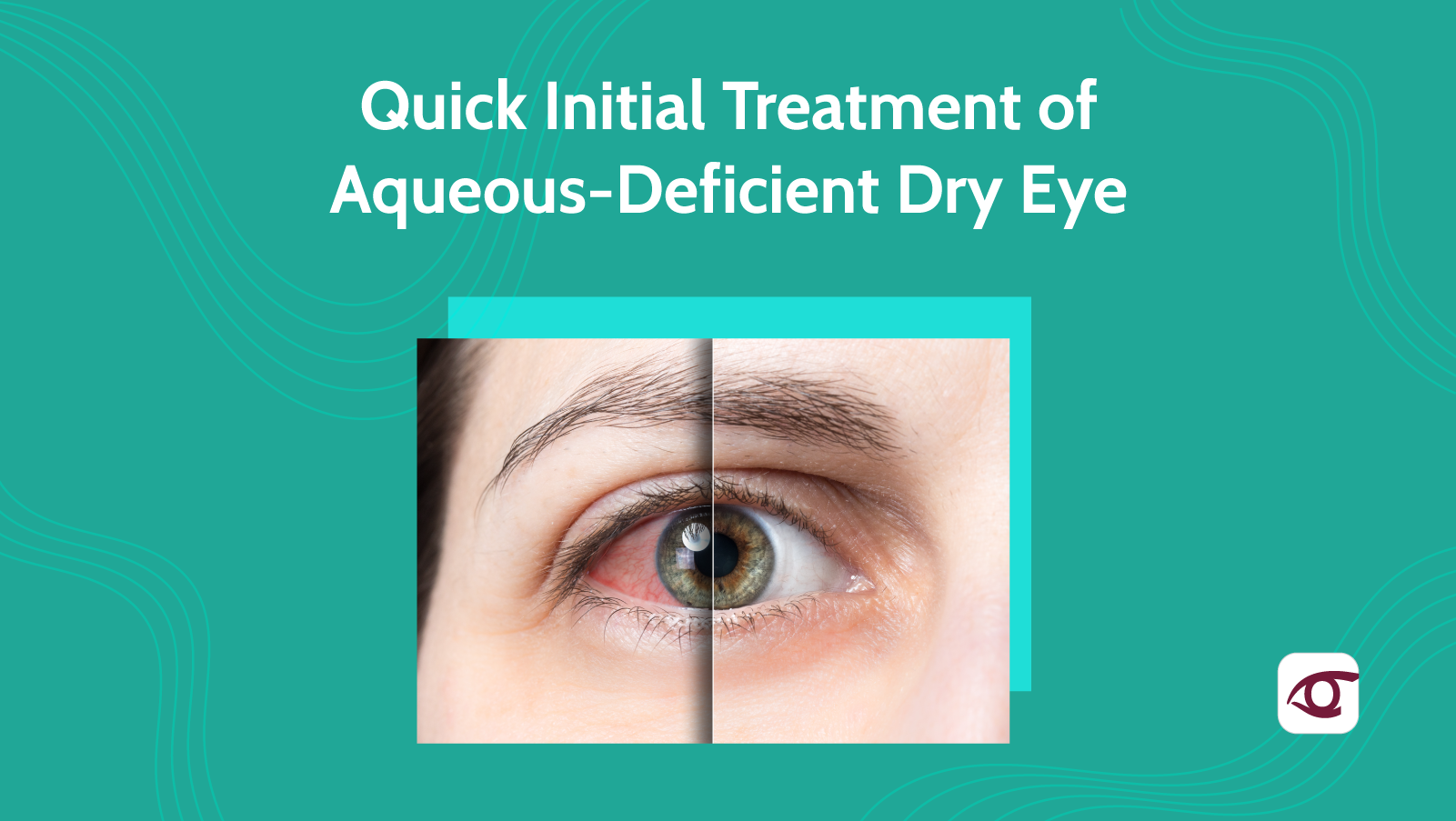
 You’ve already determined that your patient has aqueous deficient dry eye, now what? For years and years, doctors have prescribed artificial tears as a first-line treatment for aqueous-deficient dry eye (ADDE). However, in recent years, advancements in dry eye research have introduced brand new prescribing patterns for ADDE.
You’ve already determined that your patient has aqueous deficient dry eye, now what? For years and years, doctors have prescribed artificial tears as a first-line treatment for aqueous-deficient dry eye (ADDE). However, in recent years, advancements in dry eye research have introduced brand new prescribing patterns for ADDE.
Aqueous deficient dry eye can be classified as Sjögren’s syndrome (SS) and non-Sjögren’s syndrome (non-SS). SS describes an autoimmune condition that affects aqueous production in the rest of the body. It consists of an infiltration of the exocrine glands. Serological testing is indicated to determine if the patient is positive for SS. However, your treatment pattern for both SS and non-SS patients is about the same. Here are some of the key players in the treatment and management of ADDE.
Artificial tears: Artificial tears have been prescribed as a treatment for dry eye for decades. Though these drops are great at providing temporary relief of symptoms, overuse of artificial tears with preservatives can also cause corneal damage. Artificial tears can have a variety of components and formulations, so it’s important to find which one you like best for the treatment of aqueous-deficient dry eye specifically. Artificial tears can also be prescribed in conjunction with other treatments and medications, to provide immediate relief of symptoms and minimize discomfort.
Punctal plugs: The goal in the treatment of aqueous-deficient dry eye is keeping as much tear volume on the ocular surface as you can. Punctal plugs can be absorbable collagen-based or more permanent silicon-based. Punctal plugs are usually used in conjunction with other treatments.
Anti-inflammatories: Pharmaceuticals directed towards aqueous deficient dry eye have gained a lot of popularity within the past few years. However, most practitioners were initially hesitant to prescribe them given the hefty price tag. Most commercial insurances now cover most of these specialty dry eye pharmaceutical products.
Here are the top three:
- Restasis® (cyclosporine A 0.05%)
- Cequa® (cyclosporine A 0.09%)
- Xiidra® (Lifitegrast)
So what’s the difference between the two most common active ingredients? Cyclosporine A is an anti-inflammatory drug that inhibits the IL-2 activation of lymphocytes involved in the inflammatory cascade. Lifitegrast, on the other hand, has a different mechanism of action. The drug blocks the T cell from binding with ICAM-1 which may be overexpressed on the ocular surface in dry eye disease.
Steroids also play a role in aqueous-deficient dry eye treatment and management given the severity. Low dose steroids can be indicated in moderate to severe cases for fast relief of symptoms. However, steroid dosing should always be tapered when prescribed and never used long term.
In very severe cases, other forms of treatment such as autologous serum and amniotic membrane grafts are indicated. This is usually done when there is significant corneal damage or ulceration. These forms of treatment are usually reserved for when other initial treatment strategies are not successful.
Though there are plenty of other advanced methods of aqueous-deficient dry eye treatment, having a solid place to start is always key when you’re developing a treatment plan. Always remember that each patient requires a tailored treatment plan and approach depending on lifestyle and severity. Always take the time to emphasize patient compliance when beginning any treatment. Successful dry eye management always requires teamwork on the part of the doctor and the patient.
~ Dr. Amadian
